
Huntington's Disease Therapeutics Conference 2024 – Day 3
HDBuzz is back for the last day of the CHDI HD Therapeutics Conference: Thursday February 29th in Palm Springs, California. This article summarizes our real-time updates of the conference in community-friendly language. From genes to medicines The morning session will focus on how human genetics is driving the development of therapeutics. “Genetic modifiers” are genes…



HDBuzz is back for the last day of the CHDI HD Therapeutics Conference: Thursday February 29th in Palm Springs, California. This article summarizes our real-time updates of the conference in community-friendly language.
From genes to medicines
The morning session will focus on how human genetics is driving the development of therapeutics. “Genetic modifiers” are genes that influence when HD symptoms onset, and human data is extremely valuable to discover new drug targets.
Scientists can only find these modifiers when they have access to huge amounts of genetic data, so every single person from an HD family who contributed samples and signed those consent forms played an important role in all of these discoveries.
Vanessa Wheeler: expansion of CAGs and HD modifiers
The first speaker of the morning is Vanessa Wheeler, from Massachusetts General Hospital & Harvard Medical School. Vanessa’s team are experts on somatic instability (expansion of CAGs) and have been busy researching modifiers.
Vanessa is telling us about the work of a large consortium of scientists who all collaborated in a big team effort to do the best science possible. A lot of what we know about the genes that affect HD onset has come from these genome-wide association studies (GWAS). They first looked at modifiers in a very large dataset – from over 12,000 people from HD families! With such large amounts of data, they can start to parse out which modifier genes may contribute to which HD symptoms, such as movement or thinking.
The newest study highlighted familiar modifier genes, like FAN1 and MSH3, as well as a whole host of new ones, like MED15 and POLD. This is very exciting for HD researchers who are always looking for new possible drug targets or ways to alter the progress of HD. Based on this new data, Vanessa proposes a 2 stage model of HD – CAG expansion first due to faulty DNA repair, followed by the harmful effects of other proteins that mess up the normal biology of cells.
Vanessa and her colleagues at Harvard are looking to see how the human modifiers influence CAG expansions in mouse models of HD. Getting rid of these modifier genes in the mouse can have lengthening or shortening effects on CAG repeats. One of the new modifiers in Vanessa’s mouse model is a gene called HMGB1. Other HD scientists have already been working on HMGB1 because it sticks to huntingtin and plays a role in DNA repair – this is a cool connection.
Vanessa is proposing different roles for her favorite modifiers in the process of CAG repeat expansion and in other parts of HD biology. When science enters new territory, it’s interesting to hear many perspectives at global meetings like this one!
Darren Monckton: HD biomarkers to track disease progression
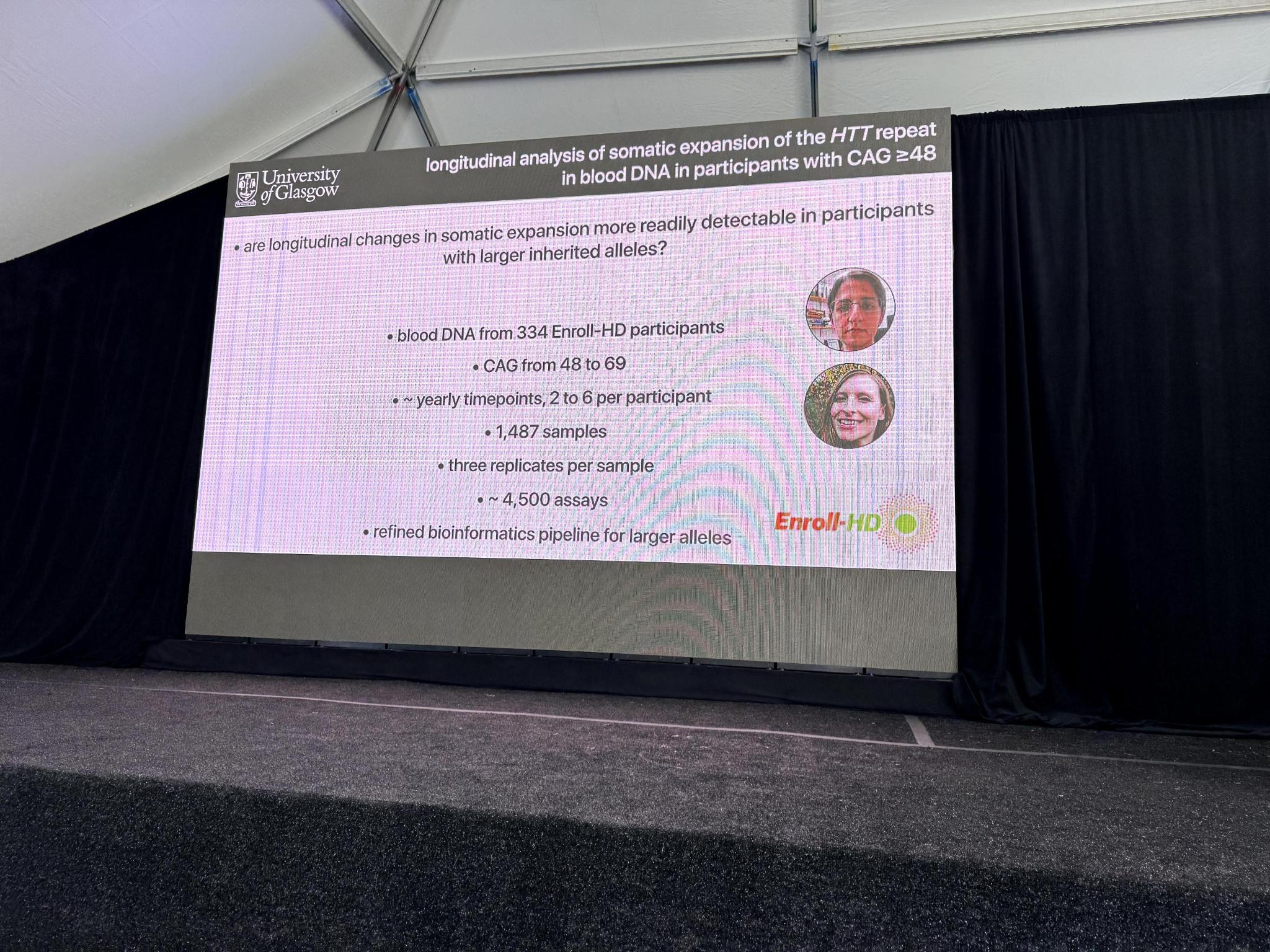
Next up is Darren Monckton from the University of Glasgow. Darren will be presenting his team’s recent work on HD biomarkers – different measurements scientists and clinicians can use to track how disease progresses over time or how it is affected by a treatment.
One of the challenges of creating drugs that combat somatic expansion is measuring whether the drug is working over time. Somatic expansion happens very slowly throughout a person’s lifetime, so how can we measure differences in a shorter timeframe, like in a clinical trial? Even more tricky is that changes in HD are happening in the brain! We can’t take out a piece of the brain to measure the effects of a drug, like we can with organs like the liver. Darren’s team have been investigating blood samples to see if this might work as a convenient, safe and reliable proxy.
Darren’s team are experts at doing very detailed analyses of the genetic code. They developed a cool technology to measure tiny changes in the CAG number which happen over time. Using blood from folks who generously donated samples to ENROLL-HD, they can see general patterns of somatic expansion as HD worsens. When they look at the level of individual people, they see there is actually a lot of variation in how their CAG numbers change.
The key thing to measure is how the CAG number changes in an individual over a reasonable timeframe, such as 1-3 years. This is not easy! To figure this all out they used a lot of different samples from the amazing and generous HD community. Darren’s team have been doing all kinds of cool science math to figure out exactly how many measurements they need to accurately and reliably detect a change in CAG number from blood samples, no matter the person’s age or initial CAG repeat number.
The most reliable measurements come from people with very long CAG repeats, such as those that cause juvenile HD. Darren and his team are working to ensure that they can make good measurements across the board, which would be important for clinical trial recruitment. Darren is also exploring these ideas in other diseases caused by CAG repeat expansions, like movement and balance disorders called ataxias.
The conference has featured so much work in the field of somatic instability. The ability to reliably measure how CAG length changes in blood, and connect it to what happens in brain, will be invaluable when research efforts lead to clinical trials.
Alice Davidson: insights from Fuchs’ disease
Next up is Alice Davidson. She’s an ophthalmologist who studies Fuchs disease, an eye disorder caused by a triplet repeat. Her work on genetic modifiers could inform HD research – it’s always fantastic to see the exchange of ideas across disciplines!
Fuchs’ disease is caused by a repeat of CTG letters in the DNA code. Alice has found that these CTGs get longer over time, just like the CAGs in HD. Her team discovered this using eye tissue donated by people with Fuchs’. Alice and her team use lots of cool technology to really get into the details of changes to the DNA code throughout the entire genomes of different Fuchs models. The CTG expansions seem to be happening in the types of eye cells that are most vulnerable in Fuchs’.
In HD, superlong CAG repeats are found in the most vulnerable brain cells. In Fuchs’, this is happening in the eyes. Similar findings about repeat expansion across different diseases lends strength to a new hypothesis that somatic instability is a major driver of symptoms. Alice’s team even found that some of the same modifier genes discovered by HD researchers seem to be coming up for Fuchs’ disease too.
Another line of research in her lab reveals that changes in the way that genes turn on and off in eye cells can also contribute to Fuchs’ disease. Some of yesterday’s talks suggest that this is also happening in HD. There are lots of interesting parallels here in techniques and findings from researchers in two different fields! The more the merrier.
Carlos Bustamante: tailored healthcare and medicines for all
“The conference has featured so much work in the field of somatic instability. The ability to reliably measure how CAG length changes in blood, and connect it to what happens in brain, will be invaluable when research efforts lead to clinical trials. ”
Carlos Bustamante, Founder and CEO of Galatea Bio, spoke about how we might work towards the possibility of tailored healthcare and medicines for all people.
Carlos starts by reminding us how powerful DNA sequencing can be and how much we’ve learned about world relationships and diseases as technologies have evolved. He also stresses the importance of diversity in large-scale human research. As we’ve heard this morning, genetic studies can lead to drug targets, but Carlos shares the statistic that about 95% of what we know comes from studying white European populations. This is not only an ethical and moral problem, but a scientific problem, if we want to make sure we have all the information needed to design drugs.
Carlos suggests that we may learn completely new things and find new paths towards therapy, if we commit to studying the genetics of more HD families in Africa and Asia, and more diverse populations in North America, South America, and Europe. He uses the example of studies in transmission of COVID-19 to show that not only social factors, but genetic factors, contributed to who was getting sick when the virus began to spread in the USA.
Galatea Bio is building a large database and biobank that focuses on a more diverse population. This is allowing them to more accurately make predictions about people’s risk factors for heart disease and other disorders, based on their genetics. Although Galatea focuses on health issues relevant to a much wider population, the HD research community can learn from this more inclusive approach to strengthen the genetic information that fuels our drug discovery pipeline.
Sahar Gelfman: how the huntingtin gene varies across a million people
Sahar Gelfman shared work from the Regeneron Genetics Center. Regeneron has been looking at how the huntingtin gene varies across almost a million different folks!
Regeneron’s approach will allow us to better understand how often the HD mutation occurs across people from different ancestries from around the world, and what range of CAG numbers they see. They are using genetic techniques and fancy statistics in lots of samples to identify when people may have been mis-diagnosed with HD and other repeat disorders. They see a similar incidence of HD and variation in CAG numbers as others have previously reported.
Although we often see HD being reported as occurring in around 1 in 10,000 people, from this study with lots and lots of data, it actually looks closer to 1 in 2000 people with 40 or more CAGs in this particular dataset. They also see higher levels of HD in folks of European ancestry. However, there aren’t a lot of samples from people outside of Europe and North America, because of historical biases and exclusion. Lots of folks are working to correct this sampling bias so we can have insight to the true numbers.
What’s happening in the clinic
The best was saved for last, with the final session covering UPDATE ON CLINICAL TRIALS!
David Margolin: uniQure’s ongoing Phase1/2 trial of AMT-130
First up is an update from David Margolin from uniQure on their ongoing Phase ½ trial of AMT-130, a gene therapy for lowering huntingtin that involves a brain surgery to deliver the drug to deep areas of the brain that are affected by HD. The drug is packaged in a harmless virus which is injected into specific areas of the brain through a well-controlled surgery. This is a one-shot therapy so folks who are treated will only have the surgery once and then their huntingtin levels should be lowered permanently.
This is exciting as it means that if this drug works, it could be a one-and-done approach. On the other hand, if things don’t pan out as we all hope, it could be bad news. Because of this, uniQure did a ton of safety testing in all sorts of HD animals and their trial in people proceeded very slowly to make sure everything was going ok.
UniQure are running two trials at the same time in the US and in Europe. Both trials are testing out a high dose and a low dose of the drug but only the US trial has a placebo arm – people who have the surgery but don’t receive the drug.
David is summarizing results from the most important question this trial will answer: whether the drug is safe and tolerable. The drug seems to generally be safe and side effects that did occur could be managed with treatment. We wrote about most of these findings back at the end of last year which you can find here: https://en.hdbuzz.net/355
UniQure next explored preliminary results asking whether the drug may have beneficial effects on slowing the signs and symptoms of HD. Things seem to look ok but it’s tricky to tell as not many folks in the trial have been on the drug very long. So we can’t expect a conclusive difference quite yet. Other measurements uniQure looked at were ok too, and there were possibly some positive effects…. However, it’s too soon to say for sure with such a small number of folks in this trial.
The key message is that nothing really bad has happened in people who received the drug. This is a big deal since this is the first gene therapy for HD to move to the clinic and we had very little idea how a one-shot therapy like this might work in people with HD. David shared that uniQure will have another update with more data in June.
Amy-Lee Bredlau: PTC Therapeutics’ update on the Phase2 trial for PTC-518
Amy-Lee Bredlau from PTC Therapeutics shared an update on a Phase 2 trial for PTC-518, a drug taken by mouth to lower huntingtin.
The oral drug that PTC is developing for HD is called a splicing modulator; this works to lower huntingtin by targeting its message copy and sending the message molecule to the cell’s trash can so the huntingtin protein is not made.
Image credit: Meghan Donaldson, HDF
Before trialing this drug in people, the PTC team tested whether it could lower huntingtin in different cell models of HD as well as in the brains of mice that model HD. They found lower huntingtin levels in the blood and in the brain – this is important as getting drugs to work in the brain can be very tricky.
The next step is to test if the drug is safe in people, which they are doing in the PIVOT-HD trial. PTC was one of the first companies to adopt the HD-ISS staging system and recruited folks into their trials in stages 2 and 3. We previously wrote about the HD-ISS staging system, which you can read about here: https://en.hdbuzz.net/325
People in the trial received either 5 or 10 mg of the drug, while some folks only received a placebo. The study is taking place across North America, Europe, and Australia. We are now seeing interim data from a small group of just 33 folks who participated in the trial. It looks like PTC-518 was pretty safe and there were no significant changes to the levels of NfL – a biomarker which tells us about overall brain health.
Importantly, they see that huntingtin levels are lowered in the blood in a dose-dependent manner – this means that folks who got more drug had more huntingtin lowering. No data was shown for whether lowering is happening in the central nervous system, such as the brain or fluid that bathes the brain, but we hope PTC will share that in their next formal update, which is promised soon.
Peter McColgan, Jonas Dorn, and Marcelo Boareto from Roche
Up next were two talks from three scientists: Peter McColgan, Jonas Dorn, and Marcelo Boareto from Roche.
Peter is starting by focusing on biomarkers in CSF, the fluid that bathes the brain. Levels of different biomarker proteins found in this fluid can give us information about different aspects of brain health. Peter and the folks at Roche are looking at these biomarkers from the spinal fluid they collected in the GENERATION-HD1 clinical trial which was sadly halted back in 2021 because of safety concerns. That trial was testing the HTT lowering drug tominersen.
Folks who received a low dose of tominersen had lower levels of huntingtin, but flat levels of NfL, YKL-40 and other markers of brain health. People receiving much more drug had more huntingtin lowering, but increased levels of NfL and brain markers indicating the brain was sick. These results have helped Roche decide on doses to use in their ongoing trial for tominersen, GENERATION-HD2, so that they get good levels of huntingtin lowering but without making brain cells sick. GENERATION-HD2 is well underway at many sites around the world, and is now more than 50% recruited.
Digital biomarkers, such as an app measuring finger tapping speed or shape drawing, allow data to be collected every day, not just when someone goes to the clinic for testing. Jonas tells about how these frequent digital biomarker measurements can give us a different picture of how folks are doing and how their disease progression might be affected by the drug.
In the future this may enable the same amount of information to be drawn from smaller groups of people so lots of different trials might take place more quickly and get us to treatments for HD faster. Jonas and the team are comparing the digital biomarkers they have measured with other traditional measures like brain imaging. They see some promising results! The data suggests these digital biomarkers are robust measures of how HD progresses.
In the Roche triple bill, we are now hearing from Marcelo Boareto, who will tell us about natural history studies. These studies don’t test the effect of a drug, but rather follow people with and without HD to see how the disease progresses as they age. Natural history studies help researchers understand what to expect in terms of changes in disease trajectory in HD clinical trials. The more we understand the normal course of HD, the better we can measure if a drug is changing the progression of HD and if it is helping folks with HD.
For many measures, people in the placebo group of GENERATION-HD1 not taking drug initially looked like they were improving. But then they proceeded to follow the same course as what we would expect from the natural history study – the placebo effect can be strong! Now that Roche has analyzed the placebo effect and how it compares to the natural disease progression, this information can be used to better design future trials to account for the placebo effect.
Swati Sathe: updates from the SHIELD-HD natural history study
Swati Sathe from CHDI shared data from SHIELD-HD, a natural history study that was initiated by Triplet Therapeutics. They were working on somatic instability but the company unfortunately closed down.
This study was designed to look at people with HD before they started to show symptoms and follow them for 120 weeks. They collected lots of different samples from the people in this study, like the fluid that bathes the brain, blood, and MRIs. The main purpose of the study was to understand how CAG repeat numbers change over time and track progression of HD with the different samples collected and tests performed. It was run in 9 sites in 5 different countries.
After Triplet closed down, the HD research foundation CHDI (which is hosting this conference) took over the study to ensure these precious samples and all of the data gathered so far would not be wasted and could be used to help inform future trials. The HD-ISS staging system was also used in this study. Incorporating it in clinical trials and natural history studies will help researchers target specific disease stages to hopefully move drugs forward faster by matching them to the people that will benefit most.
The CHDI team looked at which measurements changed over the course of the study, such as scores on movement tests, volume of vulnerable brain areas, and other metrics. They also compared their data with other studies, like TRACK-HD. The great wealth of data generated from all of the SHIELD-HD participants will inform which tests and measurements are the best ones to use over the length of a drug trial so there is the best chance of detecting whether a treatment is working.
That’s all from us for this year! The 2024 HD Therapeutics Conference was a fantastic look at ongoing trials, upcoming research, and fantastic data. We hope you all follow along next year!
For more information about our disclosure policy see our FAQ…


