
Has a "wonder drug" for dementia been discovered? (Spoiler alert: no.)
Media reports of a wonder drug for neurodegenerative diseases like Huntington's disease are overhyped
If media reports of a “wonder-drug” that could “stop all neurodegenerative brain diseases, including dementia” seem too good to be true, that’s because they are. The truth behind the headlines is that researchers tested thousands of already-licensed drugs in worms, and a couple that went on to show beneficial effects in mouse models of two rare forms of dementia. While it gives researchers two new leads, this research doesn’t prove anything about these drugs in patients with neurodegenerative diseases, and has virtually nothing to do with Huntington’s disease at all.
Studying neurodegeneration
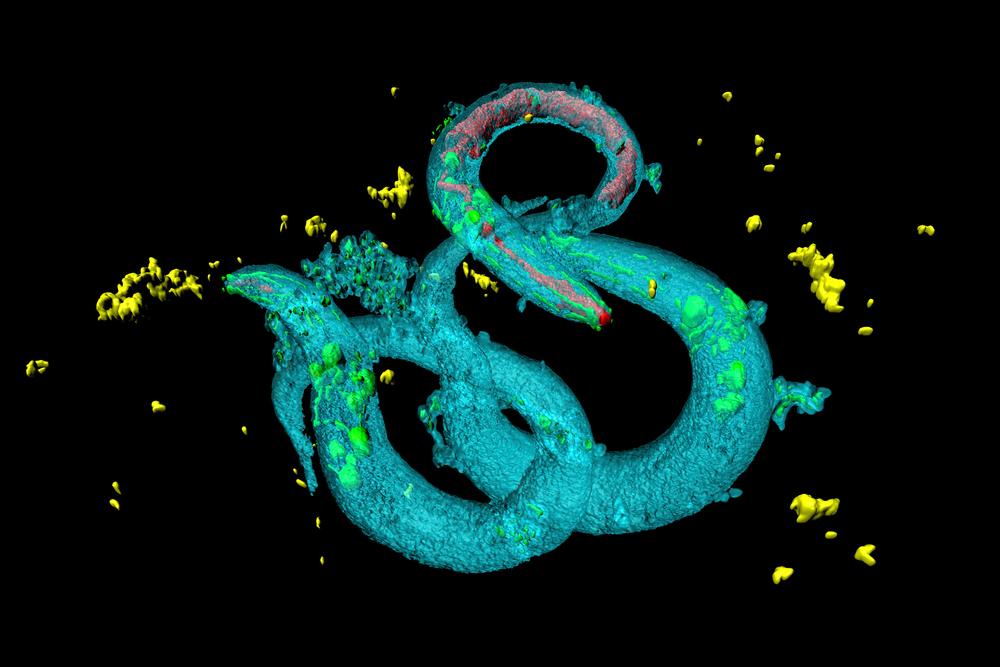
This research was led by Prof. Giovanna Malluci from the university of Leicester. Her team uses various cell and animal models to study neurodegenerative diseases, which is a term covering lots of conditions that cause neurons in the brain to die too quickly. Huntington’s is one of these, alongside Alzheimer’s, Parkinson’s and rarer conditions like prion disease (sometimes called "mad cow disease”). In lots of these illnesses, when we look at brain cells under a microscope we see that clumps of protein form. Scientists call these clumps aggregates.
How cells handle damaged proteins
Proteins are the building blocks and machinery of our cells. Proteins start as a long string of molecules, which is then folded into a complex shape. These steps are all vital for the protein to be able to work normally.
Lots of proteins end up getting damaged in the hurly burly of a busy cell. Damaged proteins are tagged, then transported to the cell’s waste recycling plant, called the proteasome, where they’re stripped down and their components used to build new proteins.
Different proteins form clumps in different neurodegenerative diseases. In Huntington’s disease, it’s the huntingtin protein, but in Alzheimer’s it’s amyloid and tau. In Parkinson’s it’s alpha-synuclein – and so on.
Surprisingly, we still don’t know whether the clumping up of proteins is something that harms neurons, or protects them from harm by hiding poisonous proteins away. It may even differ according to disease, stage and protein.
When proteins build up, it stresses cells out, so they’re evolved ways of dealing with it. One such self-defence mechanism is called the unfolded protein response. When a cell detects proteins building up, it puts the brakes on making new proteins, allowing the cell time to deal with the clump that’s already amassed. A sensor called PERK is responsible for putting the brakes on making new proteins.
This self defence mechanism is vital to help cells deal with a build up of damaged proteins.
However, in several neurodegenerative diseases, evidence from animal models suggests the unfolded protein response stays too active for too long. For all this time, the neuron isn’t making new proteins, starving it of vital machinery it needs to function properly.
Malluci suggests that this ultimately kills neurons, and reducing the unfolded protein response might be beneficial.
However, it’s important to realise we still only know a little bit about the unfolded protein response. For example, there are some diseases where it’s actually beneficial, and switching it off is bad for neurons. Already, it’s more complicated than the headlines suggest!
Drugs to tone down the unfolded protein response
“Experience tells us that success in mice is far from a guarantee of success in human patients.”
In 2013, Mallucci’s team put this idea to the test by giving the catchily-named GSK2606414 to mouse models of two neurodegenerative diseases – prion disease and fronto-temporal dementia. GSK2606414 blocks the PERK sensor – the one that puts the brakes on protein production.
This treatment restored protein synthesis in the mice, kept their neurons alive and improved symptoms and survival.
Unfortunately, whilst this was good for neurons, it turned out to be bad for other organs. GSK2606414 was toxic to the pancreas, causing the mice to lose weight and have dangerously high sugar levels, like in diabetes.
Using worms to fish for drugs
In the study that’s grabbed headlines recently, Mallucci’s team went fishing for drugs that could reduce the unfolded protein response in neurons, without poisoning other organs.
The sea they trawled was a collection of a thousand existing drugs, many of which are already licenced for use in humans, for other conditions.
The team used a technique called high-throughput screening, which involves testing lots of drugs quickly to look for a specific effect.
The ‘bait’ they used was a small worm called C. elegans. These worms stop growing when the unfolded protein response is activated. So Mallucci’s team tested to see whether any of these drugs could allow the worms to start growing again – and they found twenty drugs that did.
The next step was to check whether these drugs had their effect on the worms by the desired mechanism – namely, by reducing the activity of the PERK sensor. They made some cells in the lab that produce light when PERK is activated. Five of the twenty drugs were able to diminish the amount of light produced, suggesting that they were reducing PERK activity.
Three were discounted straight away because of side effects or because they didn’t get into the brain, leaving two potential drugs: trazodone and dibenzoylomethane (known as DBM to its friends).
The dynamic duo

Trazodone is a licensed treatment for depression and anxiety but it’s never been studied as a way to slow neurodegenerative diseases in humans. Its main side effect is sleepiness, which can be useful in insomnia, but limits its use, particularly in depression where people often already feel low in energy. It can also cause abnormal heart rhythms and low blood pressure when people stand up.
DBM is a a chemical extracted from licorice that has potential as an anti-cancer drug. It’s unclear at the moment exactly how it works. Unlike trazodone, DBM is not yet licensed for use in humans.
Testing in mice
These two drugs were then tested in mouse models of two neurodegenerative diseases – prion disease (mad cow) and frontotemporal dementia – the same mice in which GSK2606414 had looked good in 2013. The treated mice showed improved symptoms and lived slightly longer than untreated mice.
So these are wonder drugs, right?
Now we’ve explained the work in detail, you can hopefully see why we don’t think it’s appropriate for the news media, or the scientific community, to herald these two drugs as “wonder drugs”.
So far all this research has only got as far as being done in animals – worms, to be precise, followed by mice genetically engineered to show features of two rare forms of neurodegeneration.
Experience tells us that success in mice is far from a guarantee of success in human patients.
In fact, so far, no drug that slowed neurodegeneration in a mouse model has worked when tested in adult human patients.
Though trazodone has already the passed the hurdles to get licensed for depression, it doesn’t necessarily follow that it is safe and effective in patients – especially those where a mouse model hasn’t yet been tested, like Huntington’s disease.
Drugs that work in mice fail in humans for many reasons. The unfolded protein response may be very different in human brain, or may be altered differently in the various forms of neurodegeneration.
“Though trazodone has already the passed the hurdles to get licensed for depression, it doesn’t necessarily follow that it is safe and effective in HD patients”
At this point, as ever, our advice is to read about the research with a mixture of enthusiasm and skepticism. We’ve been in this situation many times before and, when scaled up and repeated, promising results have often failed to pan out. One upside is that on the whole, we are better at predicting failures in advance and avoiding them.
Enough HDBuzzkill… COULD these work in HD?
Let’s pause for a moment, turn our frown upside-down and figure out how we could show that trazodone or DBM does work for Huntington’s disease.
The first step would be to test them in a genetic mouse model of HD. There are lots of different HD mice available, and because every case of HD is caused by the same basic genetic mutation, it may be that “our” mice will turn out to be better than those of other diseases, at predicting success in human patients. However, even HD mice share that zero percent success rate, so far.
If either drug looks good in one HD mouse, it would be wise to test it again, in at least one different mouse model, to make sure the benefit is big enough and consistent across models – and also to look in the brains of the mice to make sure the drug was doing what it was supposed to do in cells.
The final step would be moving to human trials. It’s likely the regulatory agencies would give trazodone a bit of a break because it’s already widely used. But it would still need to be tested first for safety in people with Huntington’s disease, before a bigger trial to see whether it slows the disease. DBM would probably need to be fully tested from scratch.
It’s possible that somewhere, a team of researchers is already testing these drugs in HD mice, or is planning to. But even mouse research is expensive and time consuming, so these potential new leads need to be considered alongside every other treatment approach under investigation when resources are allocated.
Thankfully, the Huntington’s disease research community is well connected and well-placed to assess the whole scientific picture, not just over-hyped headlines, in deciding what drugs to test and how.
If we hear anything about this work advancing in HD, we’ll be sure to let you know. For now, in an era of “fake news”, we can draw real hope from looking beyond the headlines and exploring out together what progress is actually being made in fighting dementia and neurodegeneration.
For more information about our disclosure policy see our FAQ…


