Successful gene therapy trial in Parkinson’s Disease gives hope for HD
Success for brain ‘gene therapy’ in Parkinson’s disease – good news for similar treatments being developed in HD

Scientists have successfully used viruses to deliver genes to the brains of Parkinson’s Disease patients. The gene carried by the viruses improved the movement symptoms of patients receiving injections. This proves that gene therapy in the brain can work, providing hope for similar therapies in HD.
The connections between Parkinson’s and Huntington’s Disease
Like Huntington’s disease, Parkinson’s is a neurodegenerative condition. That means it is caused by the early death of brain cells called neurons. In some ways, the symptoms of HD and Parkinson’s might seem different – the characteristic feature of Parkinson’s disease patients is difficulty initiating movements, while the most obvious feature of HD is having too many movements. But brain circuits in the same neighborhood are involved in both diseases.

Deep beneath the convoluted outer layer of the brain (the ‘cortex’) are a set of structures called the ‘basal ganglia’. These parts of the brain are important for the regulation of movement, among other things. Different parts of the basal ganglia have opposing effects – some cause increased movement when cells in them fire, and others cause decreased movement. The part of the basal ganglia that is usually affected earliest in HD has the effect of inhibiting movement – so when it doesn’t function correctly, patients experience excess movements.
Gene Therapy versus ‘Small Molecules’
Most drugs are what scientists call ‘small molecules’. Those are simple chemicals designed to diffuse directly throughout the body and cause beneficial effects by binding to small machines in the cell called proteins. Most ‘small molecule’ drugs work by meeting the protein, and stopping the function of the protein.
It’s much easier to design drugs that stop proteins from working than to create drugs that make proteins do new things. Imagine a complex machine with spinning gears and intertwined parts. It’s easier to throw a rock into the gears and stop the machine then to add a new feature to it. So, the idea behind a lot of drug discovery is to find chemicals that stick to proteins and stop them from working.
But sometimes we know from animal models of disease that we need to make more of something happen, not less. In the case of Parkinson’s disease, it’s been shown in mice that more of a brain chemical called ‘GABA’ in part of the basal ganglia helps with symptoms. This animal finding was backed up in humans undergoing surgery for Parkinson’s – surgeons applied GABA directly to part of the basal ganglia and found that it temporarily improved the Parkinson’s symptoms.
Directly injecting GABA into the brain won’t work long-term, because the chemical is quickly used and degraded by the brain. So can we get this region of the brain to make more of its own GABA? A group of scientists and physicians decided to try to deliver a gene that instructs cells to make more GABA. If they could get this gene into this specific part of the basal ganglia, the brain would make its own GABA and that might be able to improve symptoms, as was seen temporarily when GABA was directly infused.
Delivering Gene Therapy
If it’s that easy, why not just inject the gene to tell cells to make more GABA? Unfortunately it’s not that simple. ‘Genes’ are actually made of long pieces of DNA. These are usually thousands of ‘letters’ connected in a long chain. In the case of the gene that tells brain cells to make more GABA, there’s over 3,000 ‘letters’ worth of DNA that need to get read. Getting that huge piece of DNA into cells is very tricky. If we were to simply inject DNA into the brain, very little of it would get into cells – most of it would just sit there doing nothing.
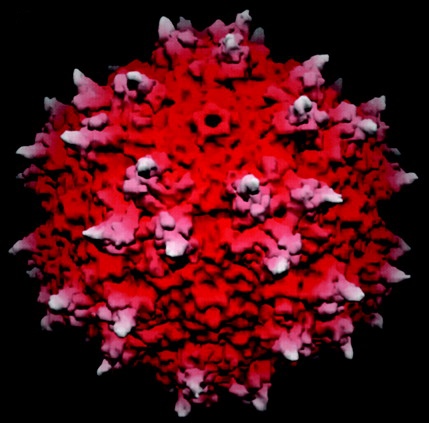
Step forward, viruses. These tiny germs are geniuses at transporting DNA from cell to cell, as anyone who’s ever had a cold knows. A virus is basically a protein package with a DNA cargo and specialist equipment for injecting that DNA into cells.
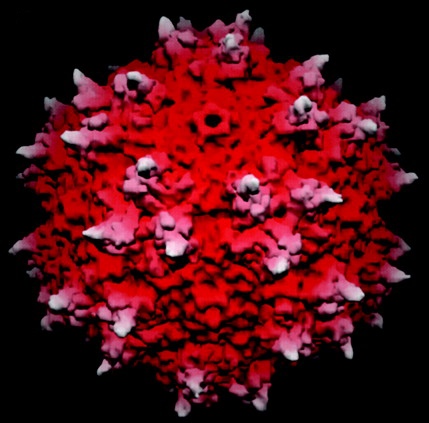
Image credit: PNAS (Xie et al)
Scientists can modify viruses so that they can’t make more copies of themselves, but are still very handy at breaking into cells and delivering a cargo of genes. By loading up these harmless viruses with the genes they’re interested in, scientists can use them to deliver any gene to regions where it’s needed. In this case, the scientists used a virus called ‘adeno-associated virus (type 2)’, filled with copies of a gene that instructs cells to make more GABA.
The neurosurgeons involved with the study then injected this ‘genetically engineered’ virus into the basal ganglia of patients with advanced Parkinson’s Disease. As a ‘control’, some patients received injections that contained no viruses. Neither the doctors or patients knew whether they had received virus.
Did it work?
After 1, 3 and 6 months all the patients in the study were assessed by a specialist Parkinson’s doctor. Patients who had received the GABA gene virus did better than those patients who received control injections – showing nearly twice the improvement in motor function. The patients will now be followed for an additional 6 months to see whether these improvements persist.
How is this relevant to HD?
Many people believe that a technique called ‘huntingtin silencing’, is the best hope to change the course of HD. One approach to this technique is called ‘RNA interference’, or ‘RNAi’. The current thinking about using RNAi in the brain is that it will require direct injection into the brain, possibly using viruses.
This Parkinson’s Disease gene therapy study targeted a brain region very close to the likely target for future Huntington’s disease gene therapy trials. The fact that the surgeons were able to target this brain region successfully, and the viruses did their job of delivering a gene, proves that gene therapy can work in the brain. That provides hope that these techniques will be useful in similarly designed Huntington’s disease trials.
Learn more
For more information about our disclosure policy see our FAQ…


