Huntington's disease goes viral as UniQure inches ahead in gene therapy race
FDA grants “Investigational New Drug” status to Huntingtin-lowering gene-therapy agent AMT-130, clearing path to human trials in Huntington’s Disease patients

Dutch-American company uniQure has received approval from the US drug regulator the FDA, to begin the first ever gene therapy trial in Huntington’s Disease. Their plan is to use a virus, injected into the brain, to turn cells into a factory that makes a weapon to lower the harmful huntingtin protein.
Huntingtin lowering recap
At HDBuzz we’re particularly enthusiastic about huntingtin lowering – a group of approaches to treat Huntington’s disease. Huntingtin lowering can be attempted using many different technologies to achieve a single goal: reduce the levels of mutant huntingtin protein in cells.
HD is caused by a mutant version of the gene that we tend to refer to as the HD gene. The gene is the root cause of HD, but the main mischief maker is the mutant huntingtin protein that the gene is a recipe for.
Our cells are constantly reading our genes to make new protein molecules. Proteins are the little machines that let cells stay healthy and carry out their jobs. But cells don’t use DNA directly as a template to build new proteins – they very carefully copy the instructions in the DNA into a closely related language, called messenger RNA, to create a temporary copy of the gene. The messenger RNA copy is then used to tell the protein-making machinery what to do.
Huntingtin-lowering aims to reduce production of the bad guy – mutant huntingtin protein. The most prominent strategies involve taking down the middle man – the messenger RNA molecule – which shuttles the genetic information from the DNA out to the protein making-machines.
Existing Approaches and News from uniQure
It’s been a time of great progress, and there are now several huntingtin-lowering drugs in clinical trials from Ionis, Roche and Wave Life Sciences. These rely on antisense oligonucleotides or ASOs – tiny bits of synthetic DNA that can recognize individual messenger RNA molecules and flag them for destruction.
In late 2017, we learned that treatment with RG6042 had lowered mutant huntingtin in the nervous system for the first time, and just this week, the first patients were enrolled in Roche’s pivotal study, GENERATION-HD1 – the first “phase 3” huntingtin-lowering trial that could lead to approval of their ASO drug RG6042 if it is proven to slow progression.
But there are other, rather different, approaches to Huntingtin lowering, and one of these got a big vote of confidence from the US Food and Drug Administration (FDA) last week. The good news came from a company called uniQure, headquartered in Amsterdam and Massachusetts. What makes their approach different is that they’re trying to lower huntingtin using gene therapy.
What makes gene therapy different?
ASO drugs like Roche’s RG6042 might be made from DNA, but that DNA isn’t permanently incorporated into the cells of the patient receiving the treatment. In contrast, gene therapy treatments involve altering human DNA or inserting new genetic instructions into human cells.
It’s a subtle distinction on paper, but one that could make a huge difference overall, because gene therapy treatments could last years or even decades, unlike ASOs or conventional drugs that have to be given again and again because they wear off much more quickly.
The most obvious gene therapy approach might be to edit our genes to remove the mutation that causes HD. That is certainly appealing, but very difficult to do safely. Instead, most companies working on HD gene therapy are trying to use it to achieve something similar to what we now know we can do with ASO drugs – take out the RNA messenger so that less of the harmful mutant huntingtin protein is made.
The problem is that every cell in the brain has the HD mutation and is making the mutant huntingtin protein every day. The aim of current HD gene therapy approaches is to turn neurons into little factories that manufacture the solution to their own problem. They do this by giving cells an extra gene that carries instructions to make a weapon to seek out and destroy the huntingtin messenger RNA. That weapon is a little piece of RNA, called a micro RNA, with a very precise design that makes it stick to the huntingtin RNA. When the cell sees the two pieces of RNA stuck together, it activates its own RNA deletion machinery to destroy them both.
Run that by me one more time

This is getting a bit complicated – so let’s recap.
The problem is a mutant HD gene that produces huntingtin messenger RNA, which tells cells to make the mutant huntingtin protein.
The solution is to add a new gene that produces another bit of RNA, the micro RNA weapon. That sticks to the huntingtin messenger RNA, causing its deletion. Less huntingtin messenger RNA means less huntingtin protein is made.
Going viral
Neurons are, by and large, not replaceable. Generally, once brain cells like this are killed, they don’t come back.
From the point of view of treating HD, this is definitely a good news / bad news situation. To date, we lack the technology to replace dead brain cells in the brains of HD patients. However, the upside is that if we can trick a neuron into becoming a drug factory for itself, we only have to do it once, since hopefully the neuron will live as long as the person carrying it around.
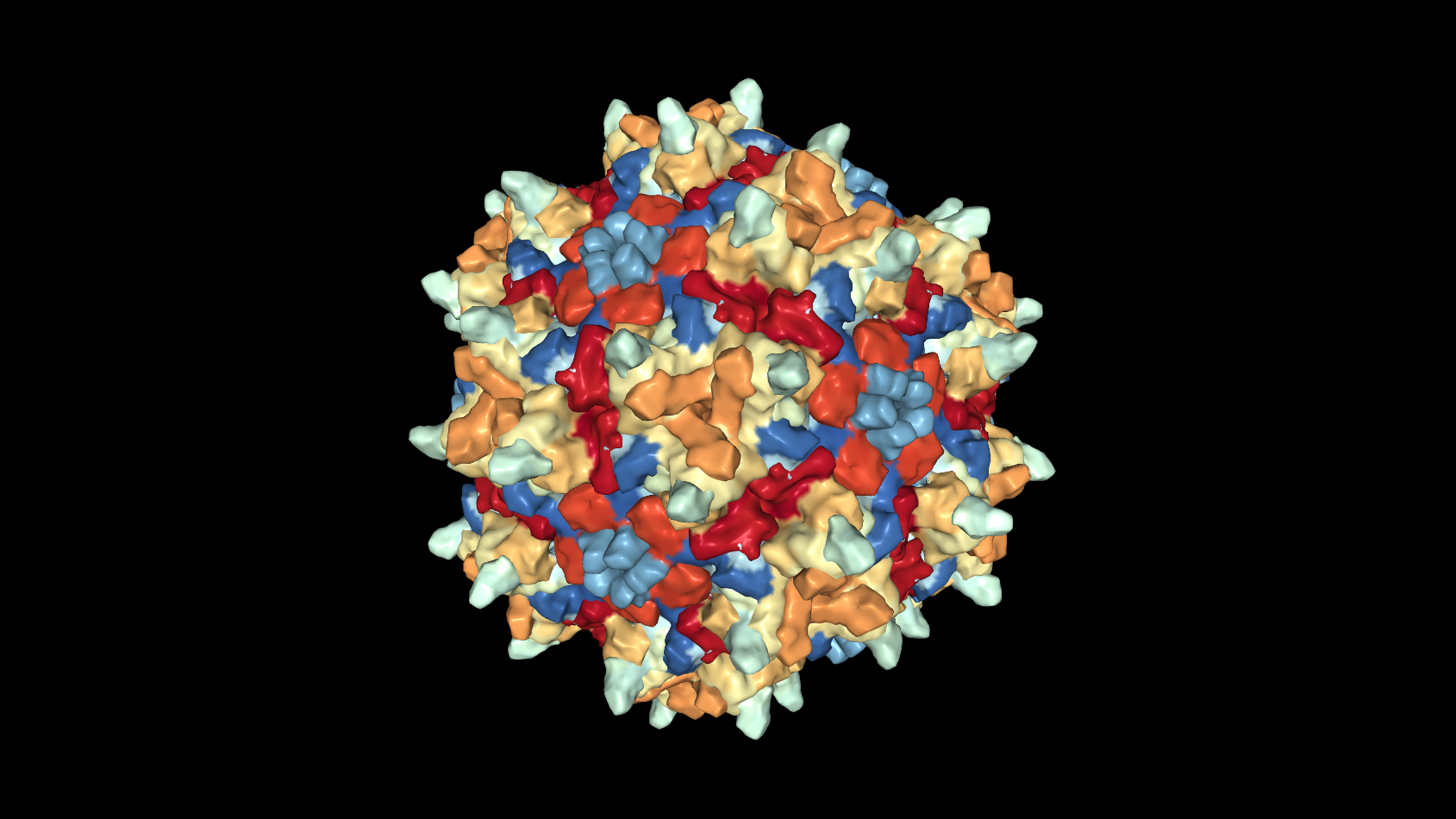
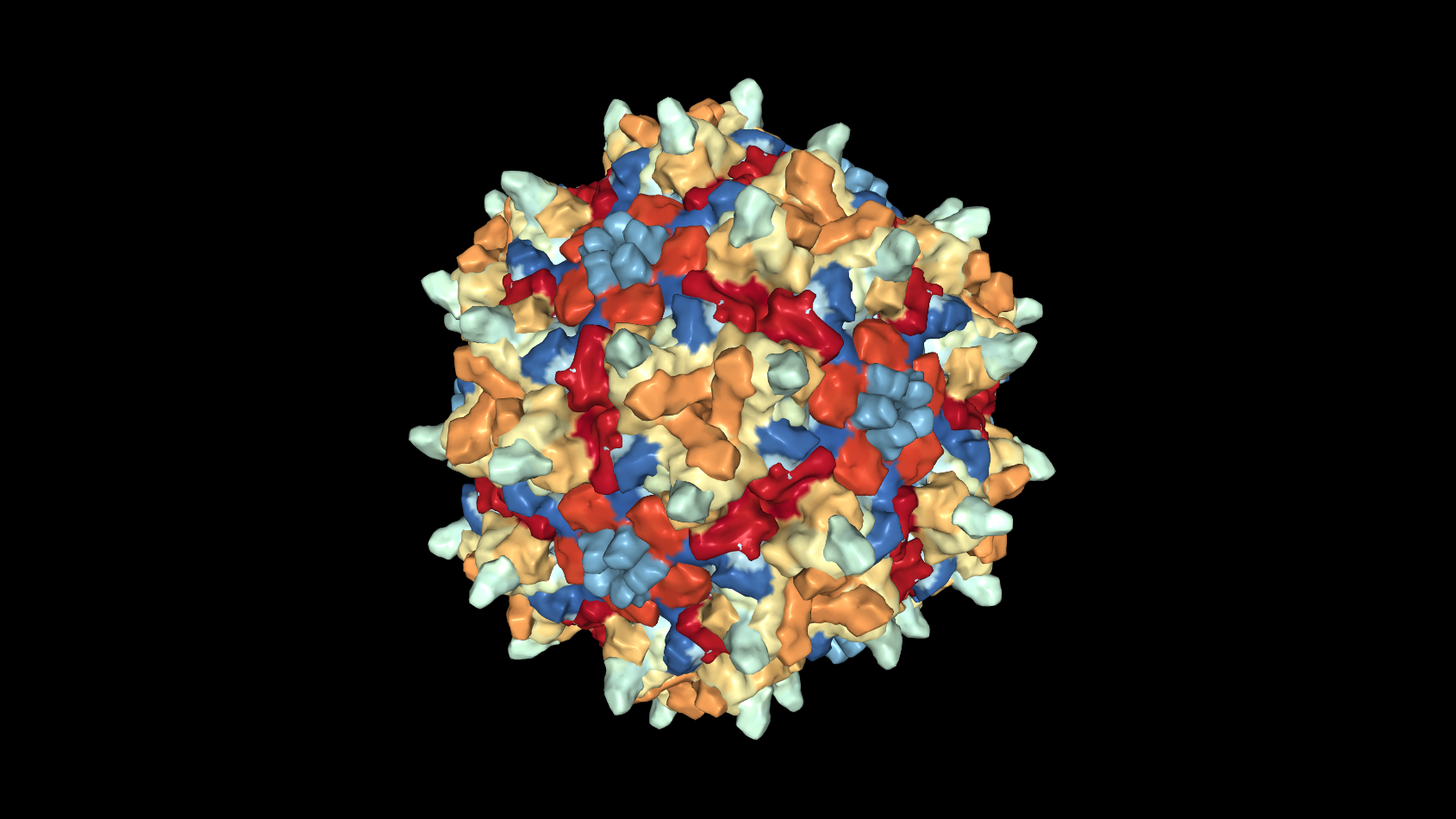
Gene therapy for brain diseases uses viruses to do just this. Researchers have worked for decades with a tiny, harmless, virus known as adeno-associated virus or AAV. Viruses have literally one goal in life – to sneak into a cell and make that cell replicate the DNA that makes more virus.
Normally this is pretty bad! However, what if we scooped out the virus’s own DNA, and instead filled it with instructions that were helpful, rather than harmful? By doing this, we could take advantage of viruses’ outstanding ability to get inside a cell and reprogram it with new DNA.
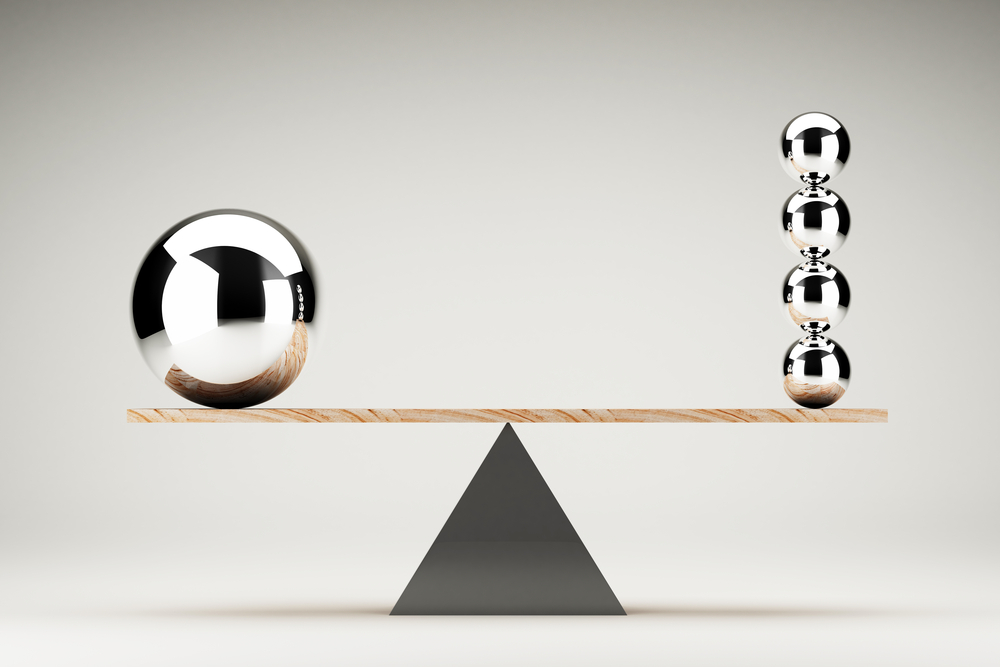
Long-lasting treatment with a single dose sounds great, but unsurprisingly there are a couple of downsides.
The first is that the virus can only get into neurons by direct injection into the brain. A neurosurgical operation would be needed to achieve this precise delivery of the viral cargo into the right part of the brain. Needless to say, brain surgery is no walk in the park.
The other main potential downside is that any side effects, as well as benefits, could be long-lasting and may be impossible to switch off.
It’s very much a high-risk, high-reward approach.
AMT-130 and IND approval
uniQure have thrown their hat into the Huntington’s disease gene therapy ring by creating an AAV virus that carries instructions for a micro RNA weapon that sticks to the huntingtin messenger RNA. The whole package – the virus and these instructions – together constitute the “drug” and are called AMT-130.
UniQure’s big announcement this week was that the US Food and Drug Administration (FDA), which regulates drugs and clinical trials, had granted AMT-130 the official status of an Investigational New Drug or IND. That’s a huge milestone in the development of any new drug and a major hurdle that has to be cleared before it can proceed to human trials. UniQure’s announcement suggests the FDA has reviewed their AMT-130 data and planned studies, and is happy for them to proceed.
IND applications are confidential, so we don’t know exactly what the company submitted. But at scientific conferences in 2018, uniQure presented data showing that AMT-130 was good at getting its genetic cargo into neurons after injection into the brain of an HD mouse, and that doing so reduced the amount of huntingtin protein they produced. Treated mice did better than untreated animals on tests of movement function, and lived longer. In the larger brains of pigs, they also demonstrated that the viral cargo spread encouragingly far, to several brain regions thought to be important in HD.
In addition to animal studies conducted by the company, an IND application will present a lot of safety data, details of how the treatment will be manufactured, and a large amount of information on the planned human studies – including the expertise of the researchers involved and how the proposedstudies will be conducted.
What’s next?
With IND status under its belt, uniQure is pressing ahead with some pretty ambitious plans.
The next step after an IND is usually for a drug company to conduct their first human studies. In HD trials, we’ve seen companies combining initial safety studies (known as phase 1) with some measurements of whether the treatment is hitting its target (information normally first collected in phase 2 studies).
Consistent with this, uniQure’s press release says “FDA clearance of the IND enables uniQure to initiate its planned dose-escalating, randomized and controlled Phase I/II clinical trial to assess the safety, tolerability and efficacy of a one-time treatment of AMT-130 in patients with Huntington’s disease. uniQure expects to open several clinical sites in the United States and begin dosing patients in the second half of this year.”
While press releases sometimes promise more than they can deliver, it’s encouraging that uniQure appears to be planning to test their drug in the second half of 2019, and clearly has a detailed plan for these initial studies. We still don’t know the exact details of the proposed study (or the locations of the study sites), but expect to learn this during 2019 as the plans develop.
Where does this leave us?
There’s a lot to process here, but overall it’s a big step in the right direction and we suggest you add this announcement to the list of things to be grateful for as we move into 2019. We started the year with two outstanding huntingtin lowering projects testing ASO drugs in patients, and now the first gene therapy approach to huntingtin lowering will likely be happening in parallel. Several other companies are working on gene therapy treatments, including Voyager and Spark Therapeutics – though none yet has the IND go-ahead that uniQure just attained.
Each approach comes with its own set of potential risks and benefits. At this stage no one knows what the best approach to huntingtin lowering will be, which is why it’s right to run all these human studies simultaneously.
It’s truly encouraging that all these companies, and the regulatory agencies, see the potential in these programs. We look forward to bringing you more exciting huntingtin-lowering news as 2019 rolls on.
Learn more
For more information about our disclosure policy see our FAQ…


