Targeting oxidative stress in Huntington's Disease
Damage to cells caused by oxidative stress is part of HD – could a new targeted drug help reduce this problem?

Some Huntington’s disease researchers believe that drugs protecting against ‘oxidative damage’ could help HD patients. Existing drugs come with some problems, so a team of scientists have tested a new drug in a mouse model of HD, with encouraging early results.
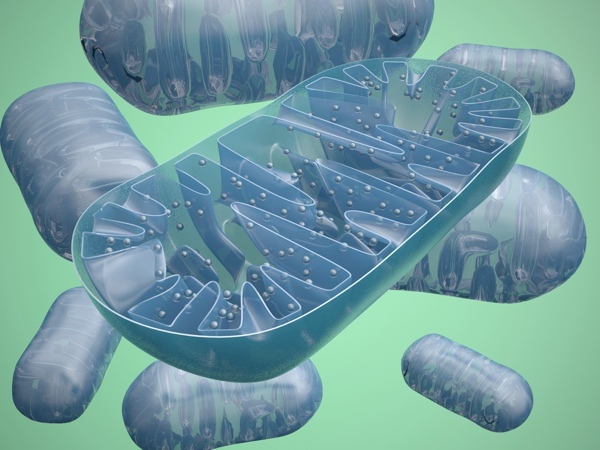
Mitochondria and oxidative stress
All cells in the body require energy to work. We consume energy-containing food, and our bodies must convert those consumed chemicals into usable energy. This process of consuming food and making energy with it is known as ‘metabolism’.

Cells from animals have an interesting way of making the majority of the energy they need to function. Tiny structures called mitochondria, which are like like miniature cells inside our cells, produce the vast majority of energy used by each cell – chewing up fat and sugar and spitting out usable energy.
But there’s no such thing as a free lunch. As a by-product of turning chemicals into usable energy, mitochondria also produce a stream of damaging, highly reactive, molecules. These molecules are called reactive oxygen species, or ROS for short, because they’re composed of different types of oxygen and are highly reactive.
We are all familiar with the damaging power of oxygen molecules, in the form of rust. Rust is a product of reactive oxygen and iron, and – can even destroy mighty machines.
Many years of evidence suggest that excessive oxidative damage is occurring in cells and tissues from Huntington’s disease patients. This has suggested to some scientists that reducing oxidative damage, using chemicals called anti-oxidants might be helpful in HD.
Problems with existing anti-oxidants
In fact, many Huntington’s disease patients already participate in trials of molecules intended to protect against oxidative stress. A nutritional supplement called ‘coenzyme-Q10’ is thought to work, in part, by serving as an anti-oxidant molecule.
Many HD patients have taken coenzyme-Q10 as a supplement, either within or outside clinical trials. The CARE-HD study, which ran from 1997 to 2000, studied the effects of coenzyme-Q10 but did not show that it was beneficial. The 2CARE study, currently ongoing, is studying Coenzyme-Q10 in the largest ever HD trial – involving over 600 participants observed over 5 years.
There is some controversy amongst scientists at how much coenzyme-Q10 gets to the brain when it’s taken in pill form. The brain is protected by a water-tight layer called the ‘blood-brain-barrier’, which blocks many drugs from entering the brain, potentially including coenzyme-Q10. Taking higher doses is one option, but that can cause increase the risk of unwanted side-effects.
‘Designer’ anti-oxidants
Because coenzyme-Q10, and other drugs like it, have a hard time getting where they’re needed, scientists have been working on developing new and improved versions of them. In 2005, the group of Valerian Kagan at the University of Pittsburgh described new and improved anti-oxidant molecules. The special feature of these drugs is that they included a chemical signal that tells the cell: “Take me to the mitochondria!”.
When these drugs get into cells they are rushed directly to the mitochondria, thanks to this tag. Having the drug there is beneficial because mitochondria generate most of the reactive oxygen species in a cell – it’s like building a fire station next to the fireworks factory!
XJB-5-131 in mice

The research group of Cynthia McMurray, at the Lawrence Berkeley National Laboratory, decided to test one of these new anti-oxidants – called XJB-5-131 – in a mouse model of Huntington’s Disease. They reasoned that this drug might help cells cope with the increased oxidative damage found in HD.
After first testing the drug in isolated brain cells, mice were injected with XJB-5-131 three times a week for over a year, to study the effect the drug had on symptoms that resemble human HD.
Like human Huntington’s disease patients, the mice used in this study lose weight and have problems with coordination. Both of these symptoms were strikingly improved in mice being injected with XJB-5-131. HD mice and humans also accumulate damage to their DNA, thanks in part to oxidative stress. Giving mice XJB-5-131 reduced this DNA damage.
Given these beneficial results, the team turned to studying directly the effects of XJB-5-131 on mitochondria they had isolated from brains of mice. They found that XJB-5-131 had a number of beneficial effects on these little powerhouses, and proposed that this is why the drug seemed so beneficial when given to HD mice.
Future directions and reservations
These positive findings in mice provide early evidence that XJB-5-131 might be worth looking at in people with HD. But, as always, there are some hurdles and reservations that are worth understanding.
In this trial, XJB-5-131 was injected into the mice, rather than being taken in the food or water. Given that this drug needs to be used for many years, taking regular injections is probably not feasible. Would a pill would be a suitable way of getting this particular drug into the bloodstream?
As we said, one of the problems with anti-oxidant drugs is that it’s not clear how much of them crosses from the bloodstream into the brain. It’s certainly not clear how much XJB-5-131 reaches the brain. This will be an important thing to work out using mice before we think about using this drug, or related ones, in people.
Finally, scientists are taught always to question their assumptions. It’s easy to think of oxidative stress as bad, which makes anti-oxidants good. But we’ve learned important things about oxidative stress, including the idea that it can sometimes be a good thing.
As an example, researchers have recently discovered that oxidative stress in muscle cells may actually help turn on many positive changes that occur after exercise. In fact, taking anti-oxidant vitamins blocked the beneficial effects of exercise in muscle tissue of human volunteers! As ever, biology has ways of surprising us with its complexity.
So, while this study of XJB-5-131 shows very compelling benefits to HD mice, mice aren’t patients, and a lot of work remains before we can know for sure how the drug was beneficial, and translate these findings into people.
Learn more
Sources & References
For more information about our disclosure policy see our FAQ…


