
A support system gone wrong – glial cells contribute to HD symptoms
An elegant new study helps determine how much brain cells called glia matter to HD symptoms
A new piece of research has implicated a type of brain cells called glia in the development of HD symptoms. Regular mice injected with glial cells carrying the mutant huntingtin gene in the study developed symptoms associated with HD. Interestingly, this influence appears to work both ways — a mild reduction in disease symptoms was seen when HD mice were treated with normal glial cells.
It’s not just about the neurons
Neurons are the cells in our brains that send electrical signals throughout our body and allow us to do all the wonderful things we can do—including reading, like you are doing now. But neurons do not accomplish this feat alone. Other cells support them and allow them to function properly. The family of glial cells is one cell group essential for proper neuron function.

Glial cells provide structural support for neurons, bring them nutrients and can fight off infections. Since neurons rely on these glial cells, it makes sense that glial cells could play a role in brain diseases like HD, which result from the early death of neurons. Recent work completed by researchers led by Dr. Steven Goldman suggests that glial cells may play a role in the development of HD and could offer new ideas about treatments.
Chimeric glia
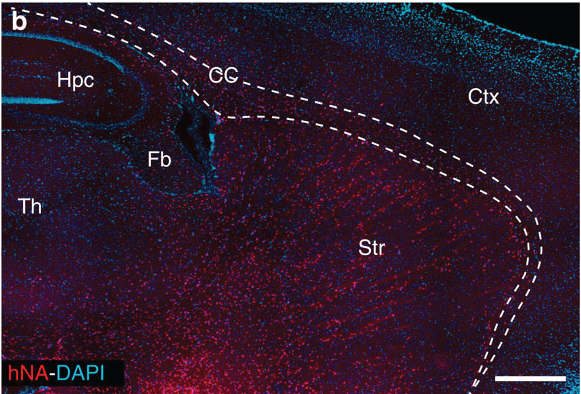
Human glial cells are more complex than those found in a mouse. Dr Goldman’s team takes advantage of this in the lab by injecting human glial cells into a newborn mouse whose immune system has been repressed. The more complex human cells out-compete the mouse cells, becoming the dominant type of glia in the adult animal.
This experiment results in the generation of what scientists call a chimera, which is an animal with cells from two species (in this case, mouse and human cells).
Exploiting the tenacity of the human glia, researchers grafted human glial cells engineered to express a mutant HD gene into newborn mice. The human glial cells replaced nearly all of the mouse glial cells. This lab trick enables researchers to study the impact of each cell type in isolation, though it wouldn’t work in the fully developed human brain, as far as we know.
Mice injected with mutant glial cells displayed some HD symptoms, including impaired coordination, as determined by rotarod test. The rotarod is basically a mouse version of a logrolling competition. Mice that had been injected with the HD glial cells fell off the rotarod before untreated mice, suggesting they were less coordinated.
Goldman’s team was interested to understand just how HD glial cells impaired the function of nearby neurons. They found that HD glia increased the excitability of the neurons, making them more likely to send messages to one another. Sort of like when a computer’s circuits become overloaded and the computer crashes, an over excited neuron can cause a bit of a ‘brain crash’.
“Exploiting the tenacity of the human glia, researchers grafted human glial cells engineered to express a mutant HD gene into newborn mice. The human glial cells replaced nearly all of the mouse glial cells”
Bottom line – mutated glial cells induced some HD-like problems with neurons that don’t have a mutant HD gene when grafted into newborn mice. This demonstrates how important glia are for the healthy functioning of neurons.
What about the other direction?
If the unhealthy glial cells could cause disease symptoms in healthy mice, the researchers then asked: can healthy glial cells rescue mice whose neurons express the mutant HD gene? Researchers investigated this question using a mouse model of HD.
This mouse model used by researchers has a severe and rapidly progressing kind of disease. Unlike human HD patients, most of who live for decades without symptoms, these mice die within a few months. For this reason, it is important to think cautiously about how these results will translate to humans—the only animal that really gets HD!
With this caution in mind, these mice do exhibit some HD-like symptoms, and so the researchers set out to determine if grafting healthy glia into newborn HD mice could alleviate those symptoms.
Modest benefits for sick mice
Normal human glial cells were injected into newborn HD mice whose immune system had been compromised. Shutting down the animal’s immune system is important to keep its body from rejecting the foreign cells being injected.
As predicted, the domineering human glial cells invaded the mouse brain and became the dominant type of glial cell. The motor skills of the HD mice that had been injected with healthy human glial cells were tested using the logrolling competition task.
At four months of age, mice that had been given the human glial cell injection could stay on the log for about 40 seconds while their un-injected counterparts could only hold on for a few seconds. An improvement, but neither group of mice stayed on nearly as long as non-HD mice (close to 230 seconds).
In addition to mildly improving motor skills, the graft of healthy glial cells slightly increased the lifespan of the mouse. As mentioned, this mouse model of HD has a rapidly progressing form of the disease — dying at about five months of age, while normal mice live around two years. On average, HD mice injected with human glial cells lived 12 days longer than the untreated mice.
This improved survival is very interesting science, but probably doesn’t live up to the headlines from news stories which suggested that “Transplants of Healthy Glial Cell Seen to Prevent Huntington Symptoms in Mice”. To truly ‘prevent symptoms’, one would expect HD mice to look like healthy mice, and these ones certainly don’t.
These breathless reports in the media can be trying for HD families. If you come across them, remember HDBuzz’s Ten golden rules for reading a scientific news story.
Other benefits from glial cell transplants
While the symptom relief caused by the injection of normal human GPCs was not dramatic, it is clear that the glial cells are worth investigating and understanding in the context of HD. In that regard, the scientists examined some of the effects of glial injections on neurons.
“The work outlined above by the Goldman group suggests that the supportive glial cells found in the brain could very well contribute to HD disease development and that glial cell replacement could be an interesting new avenue of scientific research”
Healthy glial cells caused a reduction in the excitability of neurons in HD mice. This means that the neurons would malfunction less often in those mice that had been treated, leading to a better functioning nervous system. By helping neurons relax and do their job better, glia could be keeping neurons healthy and functional for longer.
Cool science confirms glia’s importance
The work outlined above by the Goldman group suggests that the supportive glial cells found in the brain could very well contribute to HD disease development and that glial cell replacement could be an interesting new avenue of scientific research.
However, the normalization of HD symptoms after mice were treated with healthy human glial cells was fairly mild, and needs to be examined in other slowly progressing animal models before we think about trying this in people. Finally, this is a study of healthy human cells invading the brain of a newborn mouse with a severe HD mutation. It is not clear how this type of treatment would translate into human patients—more work in larger animal models is probably required before we consider human applications.
Overall, these results reveal that the role played by glial cells in HD is more interesting than scientists previously thought and it is worth investigating further to understand how they contribute the disease.
Learn more
Sources & References
For more information about our disclosure policy see our FAQ…


